As people living with chronic pain, we are experts at feeling pain, but how well do we describe it to our doctors?
As people living with chronic pain, we are experts at feeling pain, but how well do we describe it to our doctors? When I suffered damage to the trigeminal nerve on the left side of my face, I struggled to find the right words to describe the severe burning, tingling and strange sensations in my face and mouth, and the lightning bolts of pain in my eye. It sounded crazy to say: It feels like there's a sour candy stuck on the end of my tongue, It feels like I was punched in the face, It's like someone is poking my eye with an ice pick. Using elaborate scenarios like being stabbed or punched may help a family member get an idea of what we're experiencing, but can be difficult for healthcare workers to translate into medical terms. This can lead to misunderstanding symptoms and eats up precious appointment time. Learning to describe your pain using the same words medical providers use will improve communication at appointments, leading to a more accurate assessment of your condition and more time for discussing your plan of care.
Keep a Pain Journal
It shouldn't be hard to describe how you feel every day, right? When sitting in front of a doctor, it can be surprisingly difficult to give them a full picture of your pain in the short period of time allowed. Keeping a pain journal helps in many ways: records things you may have forgotten, reveals trends in symptoms that may go unnoticed, monitors the effectiveness of treatments, and quickly gives this information to your doctors, allowing more time to discuss and make adjustments to your treatment plan. Learning to keep notes using medical terms makes it easier to journal, ideally every day.
There are many aspects to address when assessing pain. Breaking them down into categories and reporting on each one gives your provider a better understanding of its nature, its cause, and how to treat it. This is especially important when your pain is coming from more than one condition, or an as yet undiagnosed source. For years, I was bedridden with severe pain. My doctors assumed it was from my neurological problems, myelomalacia, syringomyelia, and fibromyalgia. It wasn't until I had an MRI for hip pain and saw sacroiliitis as an incidental finding that I was finally diagnosed with spondyloarthritis. With accurate treatment, my pain went from a 10 to a 2-3, and drastically improved my quality of life. Careful documentation of your pain can hopefully avoid misdiagnosis or reveal undiagnosed sources.
Pain Level
In my time as a nurse doing patient assessments, the question, On a scale from 1-10, 10 being the worst pain you've ever felt, how much pain are you in now? stumped a lot of people. They had to think about what their worst pain ever was and how it compared to now. They'd tell me about the pain they had two days ago but the question is about right now. Documenting your pain level at the present moment serves as your baseline, the point by which other levels will be assessed.
For example: When beginning your journal for the day, the first pain level you note will be your baseline, and levels after that will be compared to it. This helps the doctor understand the pattern of your pain, how it responds to treatments, activity, rest, etc.
Many people have more than one chronic illness and different sources of pain. When possible, document on each pain source. For example:
!0:00AM Arthritis hip-7, knee-4. Migraine-6.
As pain levels fluctuate throughout the day, it's helpful to document these changes as much as possible. When taking pain medicine or using a treatment such as muscle rub, ice, heat, etc., document your pain level before treatment, note the treatment being used, then how your pain responds. For example:
10:00AM Arthritis hip-7, knee-4. Migraine-6. Took arthritis and migraine medicine.
12:00PM Arthritis hip-3, knee-2. Migraine-3. Heating pad-hip and knee. Ice pack-head.
1:00PM-Arthritis hip-2, knee-1. Migraine-1
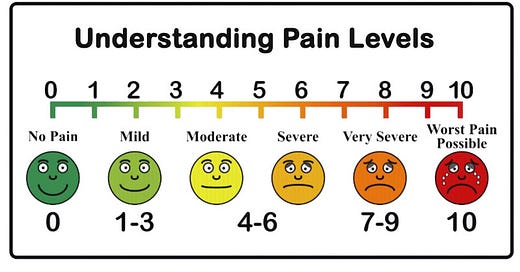
Using the Pain Scale
Pain levels are assessed using the pain scale. It can be hard to decide which frowning face or number best describes how you feel. Breaking it down into sections makes it easier to decide where your pain falls:
Normal activity to resting with an ice pack or heating pad is 1-3
Adding an over the counter pain reliever is 4-6
Adding a prescription painkiller is 7-9
If those interventions don't work, or it's a new worst pain ever , is a 10.
Once you determine which section your pain is in, it's easier to decide which of those three numbers describes it best.
Example: section 4-6, a bit more than a 4, not as bad as a 6 = 5.
Other aspects of pain are important to note to give the full picture of your condition. These should also be recorded in your pain journal:
Onset-When did the pain start? Did it happen suddenly, or has it been creeping in for a while? It's important to note if this is part of your usual pain, a new pain, or if you're not sure. It should not be assumed that a new or different symptom is from your known chronic condition.
Location-Where do you feel the pain? Is it localized-pain felt in one defined area, or diffuse-pain that is spread over a larger area and is not clearly defined. It is important to make note of this because it helps the doctor know if the pain may be referred or radiating. Referred pain tends to be spread out over an area away from its source, i.e. leg pain caused by a pinched nerve in the spine. The cause of the pain starts in the spine, but is felt in the leg. Radiating pain starts at its source and travels to other parts of the body, i.e. Low back pain from a slipped disc that extends down the leg.
Duration-how long have you had the pain? Is it new or different? Is it constant-felt all the time or for long periods, or intermittent-starts and stops.
Activity-What makes it worse? Certain movements, activities, weather, touch. What makes it better? Rest, heat, cold, medication, position, avoiding certain activities.
Timing-When does the pain occur? Is it worse when you get up in the morning and improve with activity, or get progressively worse during the day with activity? Is it worse lying down? Does it happen randomly?
Activities of Daily Living-How does pain affect your life? Does it interfere with your activities of daily living, i.e. showering, dressing, preparing meals, walking, driving, etc.
Mood/Affect-Chronic pain has a direct effect on emotional health. Reporting feelings of depression, anxiety, agitation, and other mental health symptoms is an important part of your pain assessment. If you are struggling mentally, the Suicide and Crisis Lifeline number, 988, is free and available 24/7. You can call, text, or reach them online at https://988lifeline.org or call 911.
Associated Symptoms- Reporting symptoms that may not seem related to pain is an important part of the diagnostic process: swelling, redness, numbness, weakness, tingling, burning, changes in bowel or bladder habits, dizziness, visual changes, nausea, vomiting, all can help doctors identify causes of pain.
Describing Pain
Once you've determined your pain level, it's time to decide which words best describe it. This chart from AABP Integrative Pain Care (Source: Pain Free Living (Aug/Sept 2016) describes the words commonly used by medical staff to understand pain:
Aching: A long lasting, not too serious pain. Typical of tired or injured muscle
Agonizing or Excruciating: Very Bad, you can't think about or do anything else
Burning: Like you were touching something hot. Typical of some infections
Cramping: Comes on suddenly feels like your muscle or intestine are tightening painfully.
Gnawing: Persistent dull pain similar to hunger pains.
Pins & Needles: Mildly painful feeling like you get when you sit on a foot or hand and it falls asleep
Pounding: Like something is beating on you inside.
Pressing: Like something is squeezing you or sitting on you
Radiating: Pain seems to flow from a central hurt to somewhere else, like down an arm or leg, or front to back.
Sharp or Stabbing: Comes quickly, feels like being stuck with something sharp.
Shooting: Sudden, severe pain that moves throught the body
Stiff: Usually in muscles or joints hurts to move or can't move freely
Throbbing: Gets worse and better in a rhythm, often with your heartbeat.
Tight: A body part feels like it's being squeezed.
Choosing one or two words for how your pain feels makes communication faster and easier. For example, instead of saying, It feels like I was punched in the face, I could say the pain was dull and aching. The sour candy stuck on the edge of my tongue could be reduced to tingling. Being stabbed in the eye with an ice pick is a sharp, stabbing pain.
Pain diaries can be a spiral notebook, a pretty fabric or leather-bound journal, whatever helps you consistently note your symptoms. My preference is to use the calendar app on my smartphone. I can make a note anytime, anywhere, and always have my phone with me at appointments. There are also apps for tracking symptoms. Whatever medium you choose, recording your pain and other symptoms regularly, using medical terms, is a powerful tool for managing your treatment plan with your healthcare team.





Thank you for this excellent resource. I'm sharing with my chronic illness community.
Excellent guidance! Thank you.